IVF as a treatment for couples struggling to conceive was developed in the 1970s by Sir Robert Edwards who pioneered this technique. His success in developing IVF led to the birth of Louise Brown in Oldham in 1978, who, unknown to many today, was conceived without the use of fertility drugs.
Nowadays Conventional IVF is used to suppress a woman’s natural menstrual cycle which is done by self-performed injections or taking a nasal spray for up to two weeks before starting treatment. Suppressing a woman’s natural cycle can cause menopausal side effects such as hot flushes and headaches.
Following this, the follicles (or egg sacs) in the ovary have to be stimulated to grow with stimulation drugs which can also cause symptoms such as nausea and bloatedness and occasionally a life-threatening condition called Ovarian Hyperstimulation Syndrome (OHSS).
The reason why Conventional IVF was developed was to try and obtain as many eggs as possible but it is now known that most eggs obtained by this method are abnormal and therefore will not fertilise or implant. So there is little point in putting a woman’s health at risk for no gain.
For some couples who do not want any drugs CREATE Fertility can treat you by Natural Cycle IVF in the same manner as was used before the conception of Louise Brown. This treatment aims to obtain a single egg.
The discovery of antagonist drugs has meant that it is rare to “lose” an egg so now we offer two alternatives to Natural Cycle IVF which employ antagonist drugs injections for 3 or 4 days to prevent early ovulation. Mild IVF which involves taking lower doses of FSH or HMG from Day 2 of your cycle. If your antral follicle count is low and you have a low AMH indicating low ovarian reserve you will be recommended to have Modified Natural IVF where around day 5 or 6 of your cycle you will have gentle stimulation to encourage your naturally selected follicles to grow.
To find out more about IVF with us or to book an appointment please Contact us.
IVF Step-by-Step
1. Initial Scan
The initial step in the IVF process is to undertake an advanced ultrasound scan. This scan is vital and is the key part in deciding on the treatment protocol. The imaging of the ovaries allows us to assess ovarian reserve by counting the small growing follicles called antral follicles. In addition we measure blood flow in the ovaries with Doppler which also checks fertility status.
The accessibility of the ovaries i.e. whether the follicles can be collected at egg collection will also be determined. We also check for cysts in the ovary which might affect fertility. After this, the womb (uterus) is examined to see whether the cavity where the embryo will implant is normal and the lining (endometrium) is healthy. 3D imaging of the uterus and Doppler blood flow also helps us pinpoint any physical abnormalities that may affect implantation. This assessment is performed to understand the qualitative nature of the woman’s fertility; not just how many eggs, but how healthy they are and how receptive will the womb lining be to implant an embryo. This is important for Natural and Mild IVF because it is focused on producing fewer but good quality eggs and fertilising them to produce a single high quality embryo.
No matter what treatment protocol you are on you will need to have about 3 or 4 ultrasound scans from day 5 of the cycle to assess the growth of your follicles and assess whether the endometrium is thickening up. Follicles as they grow produce oestrogen so you will have one or two blood tests to determine if the follicles are producing the appropriate levels of oestrogen. We also measure blood flow around the follicles which is almost unique to CREATE Fertility. Good blood flow brings oxygen to the egg which increases the likelihood of a high quality egg being retrieved.
3. The Trigger
When the follicles have reached 17mm or more and if the endometrium is satisfactory then an injection of a hormone called HCG is given to mature the eggs in the ovary and cause ovulation to occur 36 hours later. This means that the timing of the egg collection has to be precise so that it is retrieved before ovulation occurs.
4. Egg Collection
A woman must fast from midnight the morning before her eggs are collected. She is put under mild sedation, preventing her from feeling the procedure of egg collection. Eggs are collected under ultrasound guidance and collected with a needle. After the procedure you will quickly wake up and recover in the recovery bay. You can normally go home about 1 hour after the procedure although it is important for your partner or a relative or friend to accompany you home.
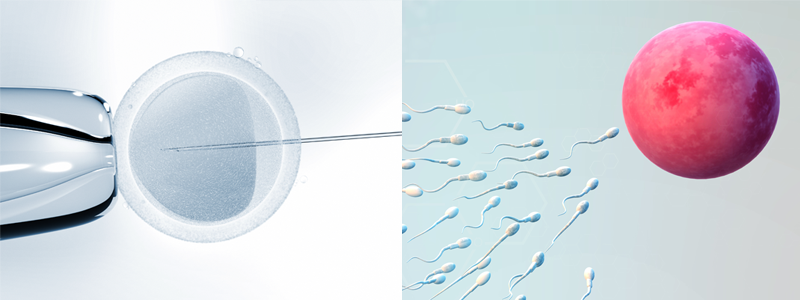
5. Fertilisation
Once the eggs are collected they are mixed with your partner’s sperm for fertilisation to occur. In some cases a technique called ICSI is used if there is a problem with your partner’s sperm such as a low count, low motility, or low number of normal forms. In this technique a normal motile sperm is injected into the substance (cytoplasm) of the egg to be used to increase the chances of fertilisation.
The eggs are then monitored for fertilisation. The woman/couple are informed the next day if fertilisation has taken place. The embryo is then allowed to develop for between 2-5 days.
6. Embryo Transfer
Once an embryo has sufficiently developed, it is ready to be transferred into the uterus. You will be in the operating theatre again. This is usually performed without sedation. Prior to embryo transfer, medication is sometimes provided to assist implantation, the medication can also continue for a number of days after the implantation period.
The receptivity of the womb for implantation differs between Natural and Conventional IVF cycles. High ovarian stimulation can thicken the lining of the womb, but this can increase oestrogen levels in the blood and negatively affect implantation. Rather than assisting with implantation, studies have shown that the implantation environment in a high stimulation IVF cycle is sub-optimal compared with a Natural or Mild IVF Cycles where the environment is more receptive to implantation and healthier.
7. Pregnancy Test
Ten days after the embryo transfer the woman has a blood sample taken for a pregnancy test. If the test is positive the woman should continue with her medication for implantation.
8. Pregnancy Scan
An early pregnancy scan is performed 2 weeks after a pregnancy test, also known as the "2 Week Wait" to confirm an intrauterine pregnancy and fetal heartbeat. A detailed report is also performed. Women are advised to book for antenatal class as in normal pregnancy with their local hospital.